A common ailment impacting a significant number of individuals in Singapore, particularly the aged, is spinal stenosis. This painful condition presents unique challenges that affect the quality of life for those contending with it.
What is Spinal Stenosis?
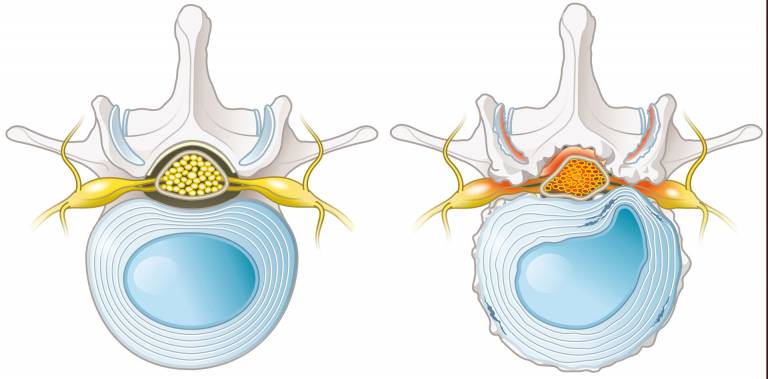
Spinal stenosis refers to the narrowing of the spinal canal, which can place pressure on the spinal cord or nerve roots. This condition commonly affects older adults and often occurs in the lower back, also known as lumbar spinal stenosis. It may develop gradually due to age-related changes such as disc degeneration, thickened ligaments, or bone spurs.
A common contributing factor is spondylolisthesis, where one vertebra slips over another, further narrowing the spinal space. Symptoms may include lower back pain, numbness, or weakness in the legs, especially during walking or standing.
Treatment options for spinal stenosis varies based on the severity and may include activity modification, physiotherapy, or medical procedures to relieve nerve compression. In some cases, spinal stenosis may require more advanced interventions such as minimally invasive surgery. Identifying the underlying cause is key to determining the most appropriate approach for managing symptoms.
What Causes Spinal Stenosis?
Spinal stenosis can result from a range of age-related and structural changes that narrow the spinal canal and place pressure on the spinal cord or nerves. Understanding the underlying cause of your spinal stenosis can help guide the most appropriate treatment approach.
Congenital Causes
In some cases, spinal stenosis is present from birth due to a naturally narrow spinal canal. Congenital spinal stenosis may not cause symptoms early on but can increase the likelihood of nerve compression as a person ages.
It can happen as a result of other conditions, such as:
– Spinal dysraphism: A developmental condition where the spine, spinal cord, or nerve structures do not fully form during pregnancy, potentially leading to structural abnormalities in the spinal canal.
– Achondroplasia: A genetic disorder that affects bone development, commonly associated with dwarfism and a narrowed spinal canal due to altered bone growth.
– Congenital kyphosis: A spinal curvature that appears at birth, where the upper back curves outward more than usual, leading to the appearance of rounded back.
Protruding or Bulging Disc
When an intervertebral disc moves out of its usual position, it can press against the spinal cord or nerves, increasing pressure on the spine. This pressure can contribute to spinal stenosis and may require spinal stenosis treatment to alleviate symptoms.
Disc Height Loss
As the discs in the spine lose height due to wear and tear, the spinal canal can narrow. Over time, this condition may worsen, potentially requiring lumbar spinal stenosis treatment or spinal stenosis surgery if symptoms become severe.
Facet Joint Syndrome
Damage or inflammation of the facet joints in the spine can cause narrowing of the spinal canal, contributing to spinal stenosis. In more serious cases, surgery may be necessary.
Bone Spur
Bone spurs, or osteophytes, form when the body produces extra bone in response to joint degeneration. These spurs can encroach on the spinal canal, leading to nerve compression and, in severe cases, may require spinal stenosis surgery.
Thickening of Ligamentum Flavum
The ligamentum flavum, a ligament in the spine, can thicken over time, narrowing the spinal canal and putting pressure on nerves. Treatment options can range from conservative lumbar spinal stenosis treatment to surgery if the condition becomes more severe.
Skeletal Diseases
Conditions like osteoporosis or Paget’s disease weaken the bones of the spine, making them more prone to fractures and deformation, which can contribute to spinal stenosis.
Space-Occupying Growths
Tumours or cysts that grow around or inside the spinal canal can physically occupy space, pressing on nerves and contributing to spinal stenosis. Spinal stenosis surgery may be needed to remove or reduce the growths.
Trauma or Surgery
In some cases, past trauma or spine surgery can lead to scar tissue or deformities that narrow the spinal canal, resulting in spinal stenosis. Additional lumbar spinal stenosis treatment or further surgery may be needed to resolve the issue.
Spinal stenosis can also be congenital (present from birth) or caused by metabolic syndromes, though these causes are rare.
Symptoms of LSS can vary based on the severity of the narrowing. It often develops slowly over time but can worsen due to trauma or physical activity. Common signs include:
- Back and leg pain, especially when standing or walking
- Pain that worsens with lumbar extension but improves with sitting or flexing forward
If you suspect you have spinal stenosis, diagnostic imaging like MRI or CT scans is used to confirm the condition.
For more information on when spine surgery might be necessary, read our article on 7 conditions that may require spine surgery.
Prevalence of Spinal Stenosis Among Singaporeans
The prevalence of lumbar spinal stenosis (LSS) is rising globally, largely due to the ageing population. In Singapore, LSS is most common among middle-aged and older adults, with a higher incidence in women. Studies suggest that between 7% and 23% of the population may be affected by LSS, and this number increases with age. For instance, around 78% of those aged 67 and older experience some form of LSS, compared to just 12% in those around 40 years old.
As LSS is increasingly recognised as a major cause of discomfort and mobility issues among older adults in Singapore, timely and effective treatment becomes essential. A local case study found that 68% of elderly patients who underwent spinal stenosis surgery had good to excellent outcomes eight years after their procedure.
If you or a loved one is dealing with LSS, don’t wait. Book a consultation with Dr Wu to explore your options for lumbar spinal stenosis treatment and potential solutions like spinal stenosis surgery.
Risk Factors of Spinal Stenosis
Ageing
Spinal stenosis is most commonly seen in adults over the age of 50. Age-related changes such as disc degeneration, bone spurs, and joint thickening can gradually narrow the spinal canal and lead to nerve compression.Physically Demanding Occupations
Jobs that involve repetitive motion, heavy lifting, or prolonged standing—such as those in construction, manual labour, or professional sports—can increase spinal stress and contribute to long-term wear and tear.Sedentary Lifestyle
Limited physical activity may weaken the core and back muscles that support the spine. Over time, this can affect spinal alignment and function, potentially increasing the risk of spinal narrowing.Obesity
Excess body weight adds pressure to the spine and may accelerate the degeneration of spinal structures, especially in the lower back. Over time, this can increase the likelihood of lumbar spinal stenosis and the need for treatment.Understanding Your Options for Spinal Stenosis Treatment in Singapore
Treatment for spinal stenosis includes a range of non-surgical and surgical approaches tailored to the individual’s symptoms, diagnosis, and daily activity levels. Spinal stenosis treatment focuses on addressing nerve compression, managing discomfort, and supporting functional movement in daily life.
Non-Surgical Treatment Methods for Spinal Stenosis
1. Activity Modification and Lifestyle Adjustments: Adjusting daily activities, avoiding symptom-triggering movements, and incorporating regular low-impact exercise may help manage mild cases of spinal stenosis.
2. Physical Therapy: Physiotherapy focuses on exercises that strengthen the core and back, improve posture, and enhance mobility. For lumbar spinal stenosis treatment, stretching and flexibility exercises may help manage lower back symptoms.
3. Medication Management: NSAIDs, muscle relaxants, and nerve pain medications may be used to manage inflammation, pain, or discomfort. These are often part of a broader treatment plan.
4. Assistive Devices and Bracing: Back braces or walking aids may be recommended to relieve pressure on the spine and provide support during daily activities. These tools can help maintain mobility during spinal stenosis treatment.
Spinal Stenosis Surgery
When non-surgical methods do not provide sufficient relief, or if there is progressive nerve involvement, spinal stenosis surgery may be considered. Common procedures include:
– Laminectomy: Removal of part of the vertebra (the lamina) to create more space in the spinal canal.
– Discectomy: Removal of part of a herniated disc pressing on a nerve.
– Spinal Fusion: Stabilisation of the spine by fusing two or more vertebrae, often used when there is spinal instability.
Minimally invasive techniques—such as endoscopic spine surgery—are available for some patients, which may reduce tissue disruption and shorten recovery time. Decisions about spinal stenosis surgery are based on the severity of nerve compression, overall health, and how symptoms affect quality of life.
Non-Surgical Treatment Methods for Spinal Stenosis
Non-surgical treatments focus on managing symptoms and improving function. Options like reducing standing or walking time, using walking aids, and taking pain relievers such as NSAIDs can help relieve discomfort. Physical therapy is also key to strengthening the muscles around the spine, offering better support. While these alternative treatments can work for many, others may eventually seek surgery for more long-lasting relief if non-surgical methods aren’t enough.
Spinal Stenosis Surgery
For those who don’t find relief from non-surgical treatments, spinal stenosis surgery may be necessary. The most common medical procedure is lumbar spinal decompression, which can be performed either through traditional open surgery or less invasive endoscopic spinal surgery. The goal is to relieve pressure on the nerves by removing thickened ligaments and enlarged joints. Endoscopic surgery is becoming more popular due to its precision, shorter recovery time, and lower risk of complications compared to open surgery.
What conditions or symptoms may indicate the need for spinal stenosis treatment?
Individuals with spinal stenosis commonly face discomfort in their buttocks and legs, affecting one or both sides. This pain intensifies when standing or walking short distances but eases when sitting or resting. Patients usually feel these sensations in the legs:
- hot or cold
- numbness
- aching
- cramps
- ant-biting feeling
The discomfort often prompts patients to reduce their walking activities and adopt a more sedentary lifestyle. In severe cases, spinal stenosis causes radiating pain in the leg and even interferes with basic functions like urination and bowel movements. Treatment is typically recommended for those encountering such symptoms.
Additionally, patients who do not experience relief from physiotherapy and pain medication may be advised to consider surgery as the next step in addressing spinal stenosis.
Lifestyle Habits To Help Prevent Spinal Stenosis
While some causes of spinal stenosis—such as age-related changes or congenital conditions—cannot be prevented, certain lifestyle habits may help reduce the risk of spinal degeneration or delay the onset of symptoms. These practices support overall spine health and may complement spinal stenosis treatment.
Stay Physically Active
Regular low-impact activities like walking, swimming, or stretching can help maintain spinal flexibility, strengthen supporting muscles, and improve posture.
Practice Good Posture
Maintaining proper posture while sitting, standing, or lifting reduces unnecessary strain on the spine. Ergonomic furniture and workspaces can also support spinal alignment.
Use Proper Lifting Techniques
Bending at the knees, keeping the back straight, and avoiding twisting during lifting can help prevent back injuries that contribute to spinal narrowing.
Maintain a Healthy Weight
Excess weight places additional pressure on the spine, especially the lower back. Managing weight through a balanced diet and exercise may help reduce stress on spinal joints and discs.
What is the Role of a Spine Doctor in Spinal Stenosis Treatment?
A spine doctor, such as an orthopaedic or neurosurgical spine surgeon, plays a vital role in treating spinal stenosis. These specialists are skilled in both surgical and non-surgical treatment options. They will assess your condition and recommend the best treatment plan for relief.
At Aspire Spine And Orthopaedic Centre, Dr. Wu Pang Hung has developed a protocol for performing endoscopic spine surgery which has been adopted by centres internationally.
We Provide Professional Help With Spinal Stenosis Treatment in Singapore
At Achieve Spine And Orthopaedic Centre, we offer specialised care for spinal stenosis, focusing on effective, minimally invasive treatments. Our experienced team provides procedures like endoscopic lumbar decompression, spinal fusion, and cervical thoracic spine surgery. We prioritise your comfort and support throughout your recovery. Learn more about spinal stenosis treatment by scheduling a consultation with us.
How Long is the Recovery Period After Spinal Stenosis Surgery?
Recovery after spinal stenosis surgery depends on the type of procedure. Dr. Wu Pang Hung’s research shows that patients undergoing minimally invasive surgery often walk within 6 to 23 hours and can go home the same day. Most can return to sedentary work after 7 days, and travel is possible within 14 days, once the wound has healed.
In comparison, recovery from open surgery with laminectomy typically takes 3 to 5 days for pain control and walking. Patients may need additional physical therapy before discharge, and recovery for sedentary work can take 4 to 8 weeks. Jobs that involve heavy lifting or strenuous activities may require 3 to 6 months for full recovery. Accordingly, endoscopic surgery offers a faster recovery, thanks to its minimally invasive approach.
What is the Cost of Spinal Stenosis Surgery in Singapore?
The cost of spinal stenosis surgery can vary, depending on the treatment options and the length of the hospital stay. Open spinal decompression and endoscopic spinal decompression are priced similarly, but the shorter recovery time and quicker discharge with endoscopic surgery can offset the higher equipment costs. In comparision, open surgery generally involves a longer hospital stay and more intensive care, leading to higher overall costs.

Wu Pang Hung
ABOUT AUTHOR
Dr. Wu Pang Hung is an experienced orthopaedic and spine surgeon in Singapore, specialising in both uniportal and biportal endoscopic spine procedures for complex cervical, thoracic, and lumbar spinal conditions. With over 10 years in the field, he is actively involved in numerous spine societies and contributes to several international journals and textbooks. Dr. Wu has also received specialised training in spine surgery across Canada, South Korea, Japan, and Germany.
Contact Us
WHATSAPP US @+65 9746 6178
CALL US @+65 9746 6178
MAKE AN APPOINTMENT
Frequently Asked Questions (FAQs)
How does physical therapy help in managing spinal stenosis symptoms?
Guided stretches and exercises will increase your strength, flexibility, and circulation. Besides strengthening and stabilising the muscles that support your spine, you’ll also improve your range of motion and balance.
What lifestyle modifications can help manage spinal stenosis symptoms?
Maintain good posture: Proper posture is key for those with spinal stenosis. Ensure your back is properly supported when you sit, and choose a chair with the proper lumbar support. Do not slouch or bend forward. Avoid standing still for extended periods, and distribute your body weight equally when standing.
Stay active: Walking, swimming, and cycling are low-impact exercises that help you build muscle, improve blood circulation, and increase flexibility. Speak with a healthcare expert to design a training program that suits your needs and skills. Do not let spinal stenosis limit you.
Strengthen your core: A robust core provides vital support for your spine. Include exercises that strengthen your core to help stabilise your spine and relieve pressure on the injured area.
Maintain a healthy weight: Being overweight puts additional strain on your spine, making spinal stenosis symptoms worse. Eat healthily and exercise regularly as part of your weight management strategy.
Create an ergonomic environment:
- Make small ergonomic changes to your surroundings to make them more spine-friendly.
- Purchase a supportive mattress to ensure your spine is properly aligned while sleeping.
- Choose an ergonomic chair with lumbar support to prevent strain on your neck and back.
Avoid prolonged standing and sitting: Prolonged standing and sitting can worsen spinal stenosis symptoms. If your work involves sitting for long periods, take regular breaks to stretch and move around. Use supportive shoes and consider using a footrest to relieve pressure on your lower back when standing for extended periods.
How does age impact the development and treatment of spinal stenosis?
Osteoarthritis, the gradual deterioration of your joints over time, is the most common cause of spinal stenosis. Since osteoarthritis starts to alter most people’s spines by the time they are 50 years old, spinal stenosis is a common condition. Because of this, most patients with spinal stenosis are 50 years of age or older.
A conservative approach should be the initial course of treatment for older patients with spinal stenosis. Reducing activity and using anti-inflammatory medications and epidural steroid injections can often relieve symptoms. Physical therapy can also help.
Are there exercises that can worsen spinal stenosis symptoms?
Yes. High-impact exercises such as sprinting, jumping, and climbing can worsen spinal stenosis symptoms. Repeated impacts to the spine from these activities can exacerbate pain.
Can spinal stenosis cause neurological complications?
Yes. Neurological symptoms include pain in the back, burning pain shooting down the buttocks and into the legs, numbness or weakness in the legs, loss of sensation in the feet, and weakness in the foot, causing the foot to slap down when walking (foot drop). Severe spinal stenosis may affect bladder and bowel control, leading to changes in urine and bowel habits.
is endoscopic spine surgery a suitable treatment for spinal stenosis?
Endoscopic spine surgery can be an effective treatment for spinal stenosis, particularly when the condition involves narrowing of the spinal canal that leads to pressure on the nerves. This procedure provides a less invasive option compared to traditional surgery, offering potential benefits such as reduced recovery time and less post-operative discomfort. However, it may not be the right choice for all patients, depending on the severity and location of the stenosis. Consulting with a spine surgeon in Singapore will help determine if endoscopic spine surgery is a good option for your specific condition.