Spinal Fusion Surgery: Risks, Benefits & Procedure
We often overlook the importance of our spine in our daily lives, realising its profound significance only when a medical condition arises. Serving as a silent pillar of support and the central axis for our body’s functions, its critical role becomes evident when pain or discomfort demands our attention.
Some conditions can lead to an instability of the spine. That’s when spinal fusion becomes a treatment option. Read on to find out just how this procedure is performed and how it’s different from other procedures.
What is spinal fusion?
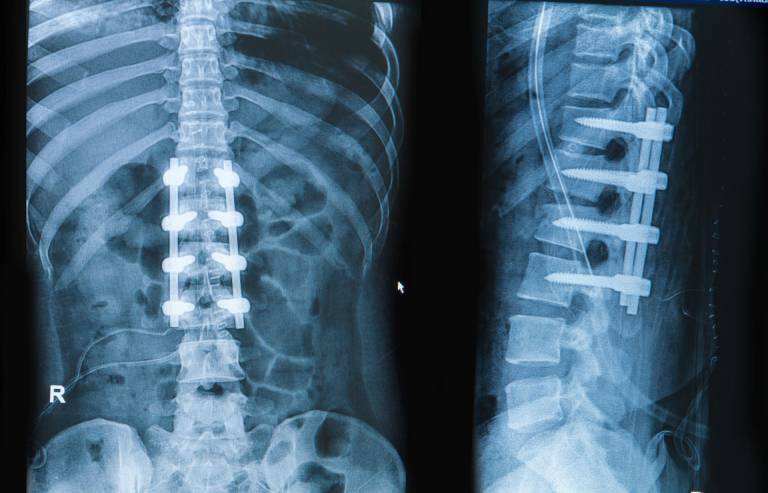
Spinal fusion is the process of permanently joining two or more vertebrae to stabilise the spine. While it may limit motion in the treated area, it can help improve spinal stability and relieve pressure on surrounding nerves.
Spinal fusion can be performed using different techniques: minimally invasive, open surgery, and, more recently, endoscopic surgery. The selected technique depends on the specific case and the patient’s needs.
What conditions can spinal fusion surgery treat?
Spinal fusion surgery is used to address specific spine conditions that cause persistent pain or instability. This includes:
- Degenerative disc disease
- Scoliosis and spinal deformities
- Spondylolisthesis
- Spinal stenosis
- Severe herniated discs
- Spinal fractures
How spinal fusion back surgery differs from other spinal surgeries
Spinal fusion back surgery aims to join two vertebrae to stabilise the spine and limit movement in that area. It’s commonly used for issues like degenerative disc disease, spondylolisthesis, and certain spinal deformities to relieve nerve compression and achieve a solid fusion of the spinal segment.
On the other hand, procedures like discectomy, laminectomy (spinal decompression), and disc replacement specifically address problems like spinal stenosis, disc herniation, and degenerative disease to maintain movement in the treated spinal area after the surgery.
What are the types of spinal fusion surgery typically performed in our centre?
Open spinal fusion
Open spinal fusion is a traditional surgical approach where a larger incision is made to access the spine. Depending on the location and type of correction needed, procedures like laminectomies, posterior fusions, and interbody fusions may be used to address degenerative spinal diseases. Although open spinal fusion surgery provides a clear view of the spine, it may also involve more post-surgical pain and increased soft tissue damage.
Endoscopic spinal fusion
Endoscopic spinal fusion is a minimally invasive surgery that uses small incisions and an endoscopic camera to guide the procedure. This technique is designed to minimise soft tissue damage while still providing spinal stability. Endoscopic spinal fusion usually results in smaller incisions, less blood loss, and shorter hospital stays.
Lateral spinal fusion
Lateral spinal fusion is another minimally invasive surgery. This procedure involves accessing the spine through the side (lateral approach) rather than the back or abdomen. By reaching the spine through the lateral part of the abdomen, the surgeon can directly approach the intervertebral disc space while avoiding major back muscles and structures. However, due to its proximity to major blood vessels and nerves, there is a slight risk of vascular injury and thigh pain.
Benefits of spinal fusion
1. Pain Management
By stabilising the spine and preventing abnormal movement, spinal fusion may help ease discomfort associated with conditions like degenerative disc disease and spondylolisthesis.2. Stability and Support
For patients with spinal instability or fractures, spinal fusion surgery helps hold the spine in place, reducing the risk of further misalignment or nerve irritation.3. Correction of Deformities
Spinal fusion may be used to correct abnormal curvature in conditions like scoliosis, helping to restore proper alignment.4. Long-Term Support
By reinforcing weakened or damaged sections of the spine, spinal fusion may help limit the chances of further complications and provide longer-term support.Potential risks and complications of spinal fusion surgery
As with any surgery, spinal fusion comes with potential risks and complications. While most procedures are completed without major issues, it is important to be aware of possible outcomes.
There are three main complications associated with spinal fusion surgery:
- Incomplete Decompression: In some cases, spinal fusion surgery may not fully relieve nerve compression, which could result in persistent pain or discomfort.
- Dural Tear: A tear in the spinal cord’s protective membrane can occur, potentially leading to cerebrospinal fluid leakage. While often repairable during surgery, it may cause temporary headaches or prolonged recovery.
- Nerve Root Injury: The nerves around the spine may be affected during spinal fusion, leading to numbness, weakness, or changes in sensation in the limbs.
Less common complications include:
- Temporary Tingling
- Postoperative Headache
- Postoperative Hematoma
- Malposition of implants and/or loosening
To help manage these risks, we use endoscopic-assisted procedures to magnify and visualise nerve structures. Additionally, our team applies irrigation techniques during spinal fusion to help reduce inflammation at the surgical site.
Recovery After Spinal Fusion Surgery
Recovery from spinal fusion surgery varies based on the individual, the specific procedure performed, and overall health. While healing times vary, following recommended recovery methods can help support the spine and enhance overall comfort during the healing period:
1. Rest and Activity Modification
In the initial recovery phase, avoid excessive bending, twisting, and heavy lifting. This will help prevent strain on the spine while healing. Increasing movement gradually, as advised by a doctor, can help restore mobility over time.
2. Pain and Discomfort Management
Discomfort is common after spinal fusion surgery. This can be managed through prescribed medication, proper body positioning, and the use of ice packs or heat therapy as recommended. Sitting and sleeping in supportive positions can also help reduce strain on the back.
3. Physical Rehabilitation and Exercises
Once the initial healing phase has progressed, specific exercises or physiotherapy may be introduced to strengthen surrounding muscles, improve posture, and support spinal alignment. These movements are typically tailored to individual recovery needs.
4. Lifestyle Adjustments
Using ergonomic chairs, maintaining good posture, and avoiding prolonged sitting or standing can help reduce unnecessary pressure on the spine. A balanced diet and maintaining a healthy weight may also contribute to long-term support.
5. Regular Follow-Ups
Routine follow-up appointments help track the recovery process after spinal fusion and identify any concerns early. Recovery timelines differ for each person, and adjustments to rehabilitation plans may be made as needed.
How does lumbar fusion differ from spinal fusion surgery?
Spinal fusion and lumbar fusion are related terms that refer to surgical procedures aimed at stabilising and fusing two or more vertebrae in the spine. The main difference is the specific region of the spine that is targeted.
Spinal fusion is a broader term that encompasses fusion procedures performed in any region of the spine, including the cervical (neck), thoracic (mid-back), and lumbar (lower back) regions.
In contrast, lumbar fusion specifically refers to fusion procedures performed in the lower back region of the lumbar spine. The lumbar spine consists of five vertebrae labelled L1 to L5.
Lumbar spinal fusion surgery is recommended for a variety of conditions, including:
- Degenerative disc disease
- Spinal stenosis
- Spondylolisthesis
- Fractures or dislocations
- Spinal tumours
- Infections of the spine
What are the potential risks and complications associated with spinal fusion surgery?
There are three main complications associated with spinal fusion surgery:
- incomplete decompression
- dural tear
- nerve root injury
Less common issues include:
- temporary tingling
- postoperative headache
- postoperative hematoma
- malposition of implants and/or loosening
To minimise these potential problems, our team uses endoscopes to examine the nervous structure closely with magnification and irrigation during spinal fusion surgery.
How long does a spinal fusion surgery typically last?
The duration of surgery depends on the condition’s complexity, the patient’s size and the choice of approach. A typical open spinal fusion takes 2-3 hours. Once the fusion device is inserted without further issues, it is expected to last the patient for their lifetime once fusion occurs 6-18 months later.
What is the cost of spinal fusion surgery in Singapore?
The cost of spinal fusion spinal surgery in Singapore differs based on the approach used, the type of implant, how long the patient stays in the hospital after surgery, and the choice of hospital and room accommodation.
For more information about the surgery cost and coverage by your insurance, it’s recommended you talk to your spinal surgeon.

Wu Pang Hung
ABOUT AUTHOR
Dr. Wu Pang Hung is an experienced orthopaedic and spine surgeon in Singapore, specialising in both uniportal and biportal endoscopic spine procedures for complex cervical, thoracic, and lumbar spinal conditions. With over 10 years in the field, he is actively involved in numerous spine societies and contributes to several international journals and textbooks. Dr. Wu has also received specialised training in spine surgery across Canada, South Korea, Japan, and Germany.
Contact Us
WHATSAPP US @+65 9746 6178
CALL US @+65 9746 6178
MAKE AN APPOINTMENT
Frequently Asked Questions (FAQs)
When is spinal fusion surgery recommended?
Spinal fusion surgery is advised for patients with conditions causing spinal instability, like spondylolisthesis and spinal deformity. Learn more about our specialised approaches to treating these conditions here.
Are there alternative treatments to spinal fusion surgery?
Yes, there are several alternatives to spinal fusion surgery, including:
Cervical/lumbar disc replacement (CDR):
- A substitute for fusion in the cervical spine.
- Relieves nerve pressure caused by disc degeneration or herniation.
Endoscopic lumbar discectomy/decompression:
- Minimally invasive technique for persistent leg and lower back pain.
- Limits collateral damage to spinal elements and soft tissue.
Coflex lumbar interlaminar device:
- Enlarges the lumbar spinal canal to provide more space for neural structures and relieve pressure from arthritic joints.
- Implants the Coflex device to offer stability without compromising mobility.
Endoscopic/fluoroscopic rhizotomy:
- It is the least invasive and most successful for chronic lower back pain related to arthritic joint structures.
- Provides pain relief for up to five years.
Intracept procedure:
- Non-invasive technique to target small neural structures responsible for pain perception from intervertebral disc endplates.
- Relieves chronic back pain in a carefully selected group of patients.
How long is recovery from spinal fusion surgery?
After open spinal fusion, standing or sitting for long periods can be challenging for the first few weeks, and it may take four to six weeks to resume light tasks. Full recovery might take six months to a year, and wearing a back brace may be necessary. However, endoscopic spinal fusion can significantly shorten this period, with recovery times almost halved. Explore further on our testimonials page.
Are there restrictions on activities after spinal fusion surgery?
Avoid activities like weightlifting, jogging, biking, or aerobics until cleared by your doctor. Refrain from driving for two to four weeks after surgery. Try not to sit in a car for more than 30 minutes during this period. For tips on post-operative care, refer to our blog.
What types of hardware or implants are used in spinal fusion surgery?
Cervical instrumentation
- Cranial screws are positioned at the base of the skull and connected to the cervical screws by rods.
- Anterior cervical plates fastened to vertebrae by bolts or screws
- Occipital plates fastened to the base of the skull by bolts or screws
- Interbody cages raise the spinal segment back to its original height following discectomy.
- Standalone cages are anchored into the bones without the need for screws or plates. These cages may lower the chance of postoperative dysphagia and hoarseness of voice.
- Cervical pedicle screws with rods (FDA-approved) are positioned at the pedicles of cervical vertebrae.
- Cervical lateral mass screws with rods are typically used from C3 to C7.
Thoracic instrumentation
- Pedicle screws with or without rods
- Interbody cages
- Lamina hooks with or without pedicle screws
Lumbar instrumentation
Many of the devices mentioned above, such as pedicle screws, rods, plates, and cages, are used as instrumentation during lumbar interbody fusion surgeries. Surgical approaches and techniques can also determine the kinds of instrumentation used in lumbar spine surgery.
ALIF: ALIF cages must be supported by plates or screw-rod structures. Large, angled cages can help the spine’s natural curve.
PLIF: Cages are used in conjunction with rods and pedicle screws
TLIF: Spacers with a potential crescent shape that are positioned in front of the disc space may be used
XLIF and OLIF: Permits the placement of a larger cage; hence, these techniques are more beneficial for treating scoliosis
How soon can I return to work after spinal fusion surgery?
Patients with office or sedentary jobs may return 4 to 6 weeks after open surgery and 2 weeks after endoscopic fusion. However, returning to more physically demanding activities may take up to 3 months. Learn more about how our advanced techniques aid quicker recovery on our Spine and Hip page.
I had previous spinal surgery before. Can endoscopic spine surgery help with revision surgery or revision fusion surgery?
Yes, endoscopic techniques are particularly beneficial for those needing revision surgery and have become more common. Revision surgery with endoscopic discectomy, decompression, and fusion techniques have several advantages.
- Lower infection risk: Minimally invasive techniques create more minor wounds and involve less soft tissue dissection, reducing the risk of wound dehiscence and infection. Continuous irrigation during endoscopic spine surgery further lowers this risk.
- Preventing durotomy: Magnified endoscopic views and lateral dissection of the dural scar tissue can be performed to reduce the chance of unintentional durotomy.
- Preserving tissue: Endoscopic vision allows for reduced soft tissue and bone dissection, preserving enough tissue to prevent instability and the need for fusion.
- Multiple approaches: Endoscopic spine surgery allows various approaches to the same target site. For example, a contralateral approach may reach the same foraminal region previously accessed through a paraspinal or transforaminal approach.
Whether you are suitable for endoscopic spine surgery as a revision surgery will depend on your condition and Dr Wu’s assessment. Discover how these methods have transformed patient outcomes here.
Will lumbar fusion surgery limit my ability to move?
Lumbar fusion surgery restricts movement in the fused section of the spine, but most patients can still perform daily activities with little impact once they have healed. The extent of mobility changes depends on the number of vertebrae fused and the individual’s overall spine health. Many people adapt to the changes over time, especially with rehabilitation exercises to maintain flexibility in the surrounding areas.
How do I know if lumbar fusion surgery is the right option for me?
Our specialists will assess your condition based on symptoms, imaging scans, and response to non-surgical treatments. Lumbar fusion surgery is typically considered when pain and instability in the lower back persist despite physiotherapy, medication, or other conservative treatments.
Is lumbar fusion considered a major surgery?
Yes, lumbar fusion surgery is classified as a major procedure because it involves permanently connecting two or more vertebrae in the lower spine. Although Achieve Orthopaedic Clinic offers minimally invasive techniques, the recovery process still requires time, follow-up care, and adjustments to daily activities.
How is lumbar fusion surgery different from other types of spinal fusion?
Lumbar fusion surgery focuses on stabilising the lower back (lumbar spine), whereas other types of spinal fusion, such as cervical fusion or thoracic fusion, target different areas of the spine. The lumbar spine bears more weight and movement, and the procedure is often used to address conditions like degenerative disc disease, spondylolisthesis, and spinal stenosis. The surgical approach and recovery process may also differ depending on the location of the fusion and the techniques used.