Endoscopic Spine Surgery
What Is Endoscopic Spine Surgery?
Endoscopic spine surgery is one of the least invasive versions of minimally invasive spine surgery. Some surgeons refer to it as the bridge between spine pain procedure and traditional open spinal surgery.
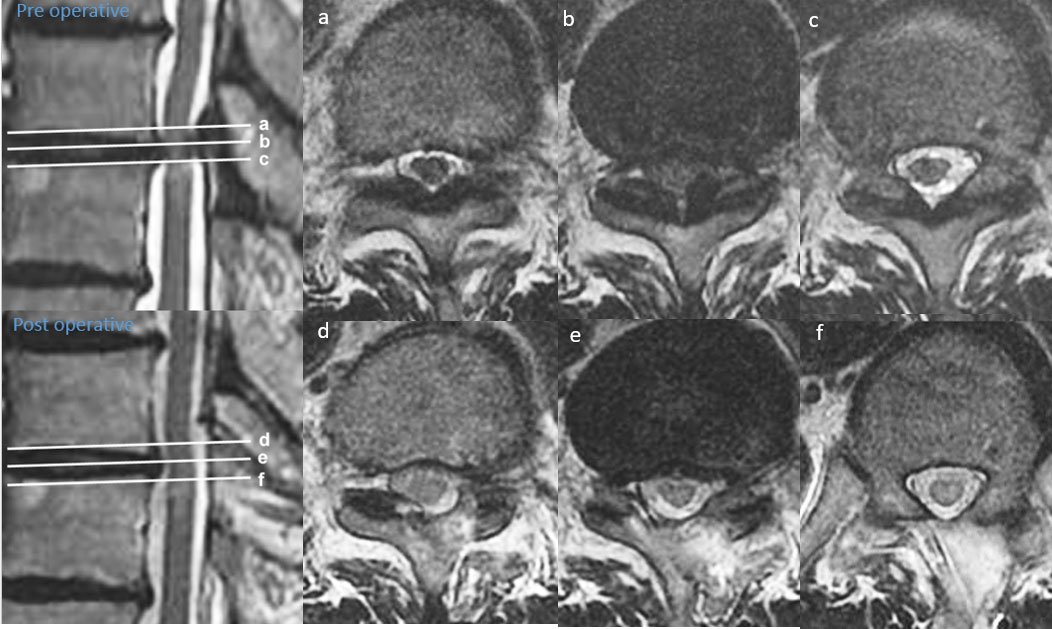
One of the procedures under this category is endoscopic discectomy, which is used to treat herniated or damaged discs in the spine. Using small incisions and an endoscope, the surgeon removes or repairs the disc material that may be pressing on nearby nerves. This approach typically involves less disruption to surrounding tissues and may result in a quicker recovery compared to traditional open surgery.
During and After Endoscopic Spine Surgery
During the procedure, the patient is typically placed under local anaesthesia, with the area to be treated numbed. The surgeon makes a small incision, usually no more than 1-2 cm, through which an endoscope is inserted. This endoscope is typically 8-10mm in diameter, and serves 4 main functions:
- Irrigation: The endoscope includes an inflow port that delivers a saline solution to irrigate the surgical site. This helps to wash away debris, blood clots, or tissue fragments, ensuring the surgeon has a clear view of the area being treated.
- Magnification: The endoscope is fitted with a camera that provides a magnified view of the spine on a screen. This enables the surgeon to work around delicate structures, such as nerves and discs, accurately and safely.
- Light Source: Light is delivered via the endoscope, eliminating the need for larger incisions while still ensuring the surgeon can see the area being operated on.
- Working Channel: The endoscope is equipped with a working channel, which is a narrow passage that allows the surgeon to pass small instruments. These instruments are used to treat the target disc, bone, or nerve region.
After endoscopic spine surgery, most patients are able to walk and may be discharged on the same day. Full recovery may take several weeks, depending on the individual case and the extent of the surgery. During this time, they should continue to follow specific post-operative care instructions, such as getting adequate rest and performing prescribed exercises.
Benefits of Endoscopic Spine Surgery
Endoscopic spine surgery has several benefits over open spine surgery. Here are the main ones:
Reduced trauma – A spinal endoscope can be inserted directly on target bony region, bypassing soft tissue to prevent repetitive trauma to soft tissue.
Minimised collateral damage – An endoscopic spine surgeon can “dock” on the target area to minimise damage to surrounding areas.
Easier access to treatment areas – As the endoscope is small in size, a doctor can fit it into spinal cavities such as the spinal foramen to perform decompression of nerves and remove a herniated disc.
Local anaesthesia – Due to the above mentioned reasons, endoscopic spine surgery can be performed under local anesthesia with moderate sedation.
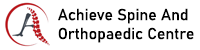
Illustrations of Endoscopic Spine Surgery


What Are the Different Types of Endoscopic Spine Surgery?
Endoscopic spine surgeries are generally divided into uniportal and biportal techniques, with a variety of procedures designed to treat specific spine issues. As surgical techniques continue to evolve, endoscopic procedures are increasingly used to treat a wider range of conditions, sometimes as day procedures, allowing for quicker recovery.
Uniportal Endoscopic Spine Surgery
Uniportal, full-endoscopic spine surgery involves a single small incision, through which the endoscope and necessary surgical instruments are inserted. This approach is commonly used for treating more focused or isolated conditions.
Biportal Endoscopic Spine Surgery
In biportal endoscopic surgery, two small incisions are made: one for the insertion of the endoscope and the other for surgical instruments. This allows the surgeon to access a larger area, making it more suitable for treating complex or multi-level conditions while still minimising damage to surrounding tissues.
At Achieve Spine and Orthopaedic Centre, we can convert up to 80% of our load of traditional open spinal surgery to endoscopic spine surgery. In selected cases, they can be performed as outpatient day surgery centre procedures, allowing patients to return home on the same day.
However, not all patients are candidates for endoscopic spine surgery. The suitability of this approach depends on the type and location of the spinal problem, as well as the patient’s overall health. Patients should have a thorough discussion with their spine surgeon to determine whether endoscopic surgery is the best option for their condition.
Conditions Treated by Endoscopic Spine Surgery
With advancements in endoscopic spine surgery, surgeons can use this method to treat damaged areas of the cervical, thoracic, and lumbar spine.
1. Cervical Spine
The cervical spine, located in the neck, consists of seven vertebrae that provide support for the neck and enable neck mobility. Damage in this area can lead to issues such as neck and arm pain, tingling, numbness, or weakness.
A common procedure used to address cervical spine issues is posterior endoscopic cervical decompression. During the surgery, the surgeon accesses the cervical spine through an incision at the back of the neck. Here, they will remove bone spurs or parts of a herniated disc compressing the spinal cord or nerve roots.


2. Thoracic Spine
The thoracic spine is the middle section of the spine, consisting of twelve vertebrae that extend from the base of the neck to the chest and abdomen. Issues in this area, such as fractures, degenerative conditions, or herniated discs, can cause pain, stiffness, or even nerve-related symptoms.
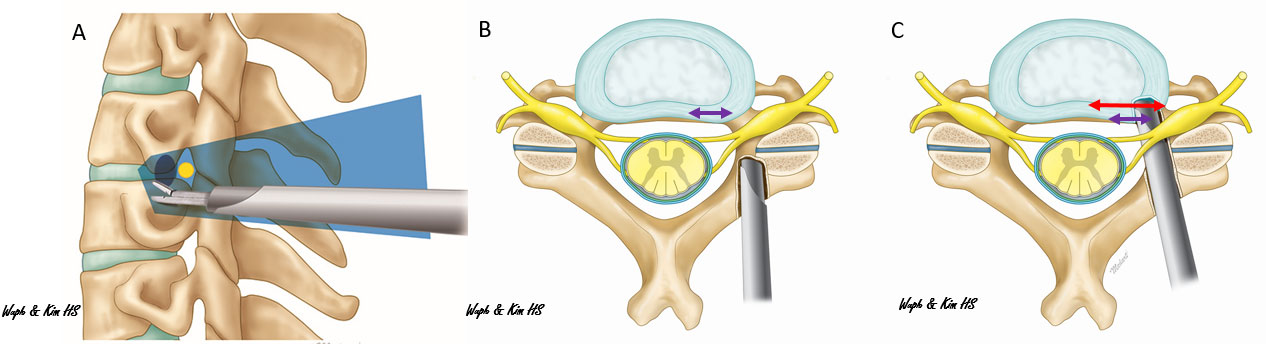
To solve these issues, endoscopic spine surgery can be a viable alternative to the traditional open chest or open back thoracic spinal decompression. (Figure 4 A and B).
In selected cases, thoracic spinal endoscopy can be performed, avoiding the need for chest opening and reducing the associated risks. However, it’s important to note that thoracic endoscopic spine surgery typically carries more risk compared to lumbar procedures due to the complexity of accessing the thoracic region. Patients should consult an experienced spinal endoscopist to determine whether this approach is suitable for their condition.
3. Lumbar Spine
The lumbar spine refers to the lower part of the vertebral column, consisting of five vertebrae. It’s located beneath the thoracic spine (mid-back) and above the sacrum (a triangular bone at the base of the spine). The lumbar spine supports the weight of the upper body and facilitates various movements, such as bending, twisting, and lifting.
The lumbar spine is the region where spinal endoscopy is most commonly performed to treat conditions such as:
- Sciatica: Pain that radiates along the sciatic nerve, often caused by a herniated disc pressing on a nerve root.
- Lumbar radiculopathy: Nerve compression in the lower back, leading to symptoms like leg pain, tingling, and weakness.
- Spinal stenosis with neurogenic claudication: Occurs when the spinal canal narrows, leading to pressure on the nerves, causing pain, numbness, or weakness in the legs.
- Spondylolisthesis: A condition where a vertebra slips out of place, leading to back and leg pain, especially during position changes or prolonged walking.
- Prolapsed intervertebral disc (herniated disc)
- Lower back pain
In our experience, close to 90% of degenerative lumbar spinal conditions can be treated with endoscopic spine surgery, with many patients able to undergo the procedure as an ambulatory day surgery
What Are the Potential Risks and Complications Associated with Endoscopic Spine Surgery?
Endoscopic spine surgery may be an option for individuals with various spinal conditions, particularly those seeking a less invasive alternative to traditional open surgery. While eligibility depends on the severity and nature of the condition, as well as individual health factors, certain groups of patients may benefit from this approach.
- Elderly Patients with Pre-Existing Health Conditions
Frail seniors or those with heart and respiratory issues who may not tolerate general anaesthesia could consider endoscopic spine surgery, as it can often be performed under local anaesthesia. - Patients with Medical Conditions That Affect Wound Healing
Individuals with conditions such as diabetes, eczema, or other skin disorders may experience delayed wound healing after surgery. The small incisions in endoscopic spine surgery offers a lower risk of wound complications for these patients. - Patients Who Require a Faster Recovery
Individuals with busy lifestyles, demanding jobs, or caregiving responsibilities may prefer endoscopic spine surgery due to its shorter downtime and potential for faster return to daily activities. - Patients Who Have Previously Undergone Spine Surgery
Those experiencing ongoing pain after prior spine surgery (failed back surgery syndrome) may find relief through revision procedures using endoscopic techniques.
Tips on Recovery After Endoscopic Spine Surgery
- Follow Post-Operative Instructions
After surgery, it’s essential to follow your surgeon’s instructions, which may include avoiding heavy lifting, bending, or twisting during the initial recovery period. - Stay Active in Moderation
Light walking and gentle movement can help prevent stiffness and improve circulation, but avoid strenuous activities or lifting heavy objects until cleared by your surgeon. - Physiotherapy
Depending on the surgery, physiotherapy or rehabilitation may be recommended to strengthen the muscles surrounding the spine and promote healing. - Rest and Hydration
Get plenty of rest and stay hydrated to aid your body’s healing process. - Monitor for Complications
While rare, complications such as infection or persistent pain may arise. If you experience unusual symptoms, such as fever, severe pain, or difficulty moving, contact your healthcare provider immediately.
Who Is a Candidate for Endoscopic Minimally Invasive Spine Surgery?
Endoscopic spine surgery may be an option for individuals with various spinal conditions, particularly those seeking a less invasive alternative to traditional open surgery. While eligibility depends on the severity and nature of the condition, as well as individual health factors, certain groups of patients may benefit from this approach.
- Elderly Patients with Pre-Existing Health Conditions
Frail seniors or those with heart and respiratory issues who may not tolerate general anaesthesia could consider endoscopic spine surgery, as it can often be performed under local anaesthesia. - Patients with Medical Conditions That Affect Wound Healing
Individuals with conditions such as diabetes, eczema, or other skin disorders may experience delayed wound healing after surgery. The small incisions in endoscopic spine surgery offers a lower risk of wound complications for these patients. - Patients Who Require a Faster Recovery
Individuals with busy lifestyles, demanding jobs, or caregiving responsibilities may prefer endoscopic spine surgery due to its shorter downtime and potential for faster return to daily activities. - Patients Who Have Previously Undergone Spine Surgery
Those experiencing ongoing pain after prior spine surgery (failed back surgery syndrome) may find relief through revision procedures using endoscopic techniques.
Can Endoscopic Spine Surgery Be Used for Spinal Stenosis?
Spinal stenosis is a condition characterised by the narrowing of spaces within the spine, which can put pressure on the nerves and the spinal cord itself. Much of our case load consists of treating this condition, from one to multiple-level spinal stenosis.
Studies show that endoscopic spine surgery can potentially preserve the facet joint better with minimal soft tissue injury. This is important in maintaining stability in the spine for patients who have experienced spinal stenosis decompression.
How Long Does an Endoscopic Spine Surgery Typically Last?
Endoscopic spine surgery, in our experience, lasts between 30 to 60 minutes per level.
At Achieve Spine & Orthopaedic Centre, our Director and Consultant Dr. Wu Pang Hung, is an internationally acclaimed spinal surgeon with a comprehensive background in endoscopic spine surgery. Dr. Wu’s dedication to advancing endoscopic spine surgery has earned him recognition from various local and overseas media outlets.
If you or a loved one are considering endoscopic spine surgery in Singapore, consider scheduling a consultation with Dr. Wu to take the first step towards a pain-free life.
What is the Cost of Endoscopic Spine Surgery in Singapore?
The approach and equipment used in each procedure vary. You will need to discuss with your endoscopic spine surgeon to find out what meets your needs and the cost that will be incurred.

Wu Pang Hung
ABOUT AUTHOR
Dr. Wu Pang Hung is an experienced orthopaedic and spine surgeon in Singapore, specialising in both uniportal and biportal endoscopic spine procedures for complex cervical, thoracic, and lumbar spinal conditions. With over 10 years in the field, he is actively involved in numerous spine societies and contributes to several international journals and textbooks. Dr. Wu has also received specialised training in spine surgery across Canada, South Korea, Japan, and Germany.
Contact Us
WHATSAPP US @+65 9746 6178
CALL US @+65 9746 6178
MAKE AN APPOINTMENT
Frequently Asked Questions (FAQs)
What is the recovery time after endoscopic discectomy?
Recovery times vary, but most patients can walk within 4 to 6 hours after surgery and resume light activities within a few days. Full recovery and returning to normal activities typically takes 3 months, depending on the individual’s condition and adherence to post-operative care.
Is endoscopic spine surgery painful?
Endoscopic spine surgery is designed to be minimally invasive, resulting in less post-operative pain compared to traditional open surgery. Patients may experience mild soreness or discomfort, which is usually manageable and tends to improve within a few days.
How long does an endoscopic discectomy take?
Depending on the severity of your condition, an endoscopic discectomy usually takes between 1 to 1.5 hours. Most patients are able to go home on the same day.
How do I know if I need endoscopic spine surgery?
You may be a candidate for endoscopic spine surgery if you have a spine condition, such as a herniated disc or spinal stenosis, that causes persistent pain, numbness, or weakness. A consultation with a spine specialist can help determine if this option is right for you.