As we grow older, it is inevitable for our bodies to change. But one area is particularly prone to age-related issues, and that is our spine. Many older adults experience some form of back pain or discomfort, which can greatly impact their mobility and overall well-being if left unaddressed.
In this guide, we will delve into some of the most common spine problems in older adults, how these conditions develop, and how minimally invasive treatments can improve recovery outcomes.
Common Spine Problems in Older Adults
Degenerative Disc Disease (DDD)
Degenerative disc disease is a leading cause of spine problems in older adults, affecting more than 90% of individuals over 60 years old. It occurs when the intervertebral discs, which are the spongy cushions between the vertebrae, gradually lose their elasticity and water content. This natural wear-and-tear process reduces the discs’ ability to absorb shock, which can cause discomfort and limit spinal mobility.
What Causes DDD?
While DDD is largely due to ageing, certain lifestyle habits and other factors can exacerbate it.
Genetics
There is existing research that suggests that individuals with certain genetic predispositions may be more likely to develop age-related spine conditions. For example, individuals with variations in the vitamin D receptor (VDR) gene, which plays a crucial role in regulating calcium absorption and bone metabolism, are more likely to suffer from DDD.
Lifestyle Factors
Everyday habits and routines have a profound impact on spine health, especially as we age. Prolonged poor posture, such as slouching while sitting or standing, places unnecessary strain on the spine and accelerates the wear on intervertebral discs. A sedentary lifestyle may also increase stress on the discs by weakening the core and back muscles that provide essential support for the spine.
Stages of Degenerative Disc Disease
1. Dysfunction
At the onset of DDD, subtle changes occur in the spine that are often painless and go unnoticed. During this stage, the discs may develop minor tears or weaknesses, leading to slight imbalances in the spine’s alignment or curvature. These changes can begin to affect posture and, over time, place mild pressure on nearby nerves, setting the stage for future symptoms.
2. Dehydration
As the degeneration progresses, the discs lose their ability to retain water, becoming dehydrated and less elastic. This not only makes the disc less effective at absorbing shock but also makes it thinner. Over time, the reduced disc height can result in increased pressure on surrounding vertebrae and joints and lead to instability in the spine.
Symptoms during this stage may include more consistent back pain, stiffness, and occasional nerve irritation, particularly after prolonged activity or standing.
3. Stabilisation
In response to the ongoing degeneration, the body attempts to stabilise the affected area of the spine. Bone spurs (osteophytes) may form along the edges of the vertebrae, reducing spinal flexibility and compressing nearby nerves. This may result in chronic pain, tingling, or weakness in the limbs.
4. Collapse
By the final stage, the discs will have significantly deteriorated. Without the cushioning effect, the vertebrae may grind against each other, causing severe pain. In some cases, the spine may become so unstable that the body initiates a natural fusion process, where adjacent vertebrae grow together. Surgical interventions, such as spinal fusion or disc replacement surgery, may be needed to stabilise the spine and reduce pain.
Other Spine Conditions Caused By DDD
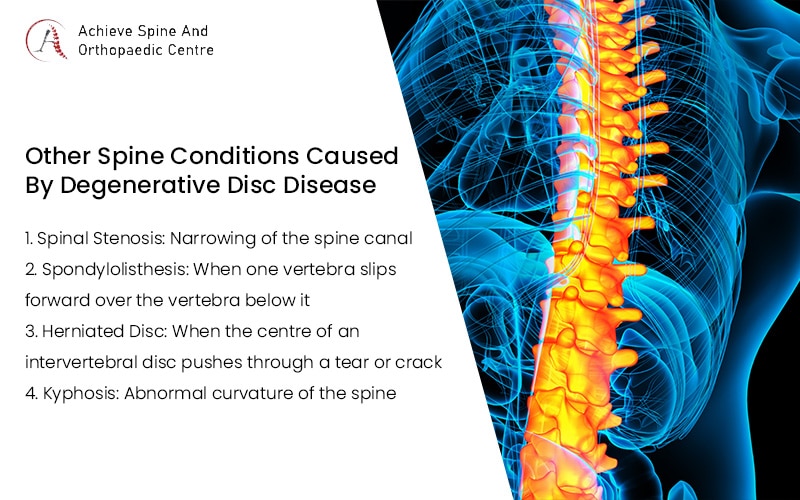
DDD does not only cause localised pain and discomfort; it can also lead to or exacerbate a range of other spine problems in older adults. When the structure of the spine is compromised, it may trigger a domino effect of issues.
1. Spinal Stenosis
Spinal stenosis refers to the narrowing of the spinal canal, the space that houses the spinal cord and nerves. As the discs in the spine degenerate, the gaps between vertebrae shrink, and the surrounding ligaments and bones may thicken, further reducing the space within the canal. This causes compression of the spinal cord or nerve roots, leading to painful symptoms.
Although spinal stenosis can occur anywhere along the spine, it is most commonly seen in the lower back (lumbar region). Studies show that around 21% of individuals over the age of 60 experience lumbar spinal stenosis.
Symptoms
- Pain in the lower back, legs, or arms.
- Numbness or tingling that worsens with prolonged walking or standing.
- Weakness in the legs, making movement more difficult.
Treatment
Lumbar spinal stenosis treatment often begins with conservative, non-surgical approaches, such as physical therapy, anti-inflammatory medications, or spinal injections.
However, for individuals with severe symptoms or those who do not respond to conservative surgical treatments, minimally invasive procedures may be recommended. Spinal decompression surgery, for example, aims to relieve pressure on the nerves by removing the bone, ligament, or disc material that is narrowing the spinal canal.
2. Spondylolisthesis
Spondylolisthesis occurs when one vertebra slips forward over the vertebra below it, causing instability in the spine. This condition can lead to significant discomfort and further spinal misalignment.
The most common type is degenerative spondylolisthesis, which is closely associated with DDD. Other types include congenital (present at birth), isthmic (caused by a stress fracture in the vertebra), and traumatic (resulting from an injury or accident).
Symptoms
Older adults with this spine problem may experience:
- Lower back pain
- Sciatica, where pain radiates down the leg.
- Leg pain, numbness, or weakness, especially when walking or standing for prolonged periods
- Difficulty walking, standing, or maintaining posture
3. Herniated Disc

As discs undergo degeneration, they become more vulnerable to herniation, particularly when under stress from activities like bending, lifting, or twisting. This occurs when the soft, gel-like centre of an intervertebral disc pushes through a tear or crack in the outer disc wall. This may compress nearby nerves and cause significant pain and discomfort.
Symptoms
Herniated discs often cause localised pain and discomfort, along with radiating pain, numbness, tingling, or weakness in the arms or legs. Symptoms tend to worsen with activities that involve bending, lifting, or sudden movements. In some cases, herniated discs can cause chronic pain that significantly impairs daily function.
4. Kyphosis
Kyphosis refers to an abnormal forward curvature of the spine of 50 degrees or greater, often leading to a hunched or rounded back. As people age, the risk of developing kyphosis increases due to the natural loss of bone density and the degeneration of spinal discs. As a result, this spine problem is fairly common in older adults, affecting approximately 20–40% of individuals.

Symptoms
The most noticeable symptom of kyphosis is a rounded upper back, often leading to a visible hump. In some cases, individuals may also experience stiffness in the back, discomfort, and difficulty with activities like bending or reaching. In severe instances, kyphosis can affect the chest and lungs, leading to difficulty breathing.
Effective Treatments and Approaches for Spine Problems in Older Adults

Having explored the common spine conditions in older adults, it is time to consider the various treatment options available. However, treating spinal degeneration in seniors calls for a more careful and personalised approach that takes into account their health, mobility goals, and risk tolerance.
Key Considerations for Older Adults
1. Health and Medical History
For older adults, medical conditions, such as diabetes, cardiovascular disease, or osteoporosis, can influence how the body responds to surgery or recovery. For example, diabetes can slow down the healing process, while cardiovascular conditions may increase the risk of complications during anaesthesia. A qualified spine surgeon should thoroughly assess their older patient’s health history to tailor treatments that minimise risks and improve outcomes. They should also ensure that any underlying conditions are managed appropriately during the treatment process.
2. Mobility Goals
When treating spine problems in older adults, the focus should extend beyond pain relief to improving functionality and promoting independence. Spine issues often hinder daily activities such as walking, lifting, or sitting for long periods, greatly impacting quality of life. That is why rehabilitation and physical therapy are essential components of the treatment plan. These help seniors regain strength, balance, and coordination, ultimately enhancing their mobility and supporting a more active, independent lifestyle.
3. Recovery Time
As we age, the body’s ability to heal slows down, and elderly patients may take longer to recover from surgery or conservative treatments. This slower recovery process needs to be factored into the treatment plan to ensure it aligns with the patient’s physical capabilities. It is important to set realistic expectations and provide appropriate post-surgery rehabilitation.
4. Surgical Risks
Even with modern surgical techniques, open spine surgery carries potential risks that should be carefully considered, particularly for older patients. Common complications include infections, blood clots, anaesthesia-related issues, and slower recovery due to the body’s natural ageing process. Additionally, pre-existing health conditions, such as obesity or poor circulation, can increase the likelihood of complications during and after surgery.
For the safest possible outcome, seniors must undergo a thorough pre-surgical evaluation. This helps to assess the risks and benefits of surgery, allowing patients and their families to make informed decisions about their treatment. They will also need to be closely monitored throughout the recovery process in order to quickly address any issues that may arise.
Introducing Minimally Invasive Spine Surgery
Minimally invasive spine surgery (MISS) has emerged as an increasingly popular treatment option for older adults dealing with spine problems. Some of their advantages are:
1. Smaller Incisions and Less Pain
Minimally invasive procedures like endoscopic spine surgery use small incisions (often less than an inch) compared to the much larger cuts required for traditional spine surgeries. These smaller incisions not only result in less visible scarring but also minimise damage to surrounding muscles, ligaments, and tissues. This also results in less post-operative pain. The reduced disruption to soft tissues also means there is less muscle strain, which can decrease the need for strong pain medications.
2. Reduced Surgical Risks
With the smaller incisions and less invasive nature of MISS, there is a significant reduction in surgical risks. Additionally, many procedures can be performed under local anaesthesia. This further lowers the risks associated with general anaesthesia for elderly patients, including issues like cognitive dysfunction and complications related to immobility. Furthermore, the reduced trauma to surrounding tissues contributes to lower infection rates, which is particularly important for elderly patients whose immune systems may be compromised or slower to respond.
3. Shorter Recovery Time
One of the main benefits of MISS for spine problems in older adults is the quicker recovery time it offers. Traditional open surgery usually involves a lengthy stay in the hospital and more time spent recovering. Conversely, MISS allows most patients to start walking within just a day and return fully to their daily routine in six weeks.
4. More Cost-Effective
While the cost of MISS can vary, it can become more affordable in the long run compared to traditional spine surgery. Smaller incisions and faster recovery times generally mean shorter hospital stays and fewer complications, both of which can help reduce overall treatment costs. Additionally, since patients often need less rehabilitation time, the costs associated with recovery can be lower.
However, it is important to note that not all spine conditions can be treated with minimally invasive techniques. A thorough evaluation by a spine specialist will be essential to determine the best treatment approach for your specific needs.
Frequently Asked Questions About MISS for Spine Problems in Older Adults
1. How does MISS compare to traditional open surgery in terms of cost?
Although the initial cost of MISS may be comparable to traditional open surgery due to the novel equipment used, it can be more cost-effective in the long term. With shorter hospital stays, faster recovery, a reduced need for medication, and fewer complications, some patients may be able to enjoy lower overall treatment costs.
2. Will I need to make any lifestyle changes after my surgery?
Just like with any surgery, patients are often advised to avoid heavy lifting, bending, or twisting for a period of time to ensure proper healing. Your doctor may also recommend specific exercises or physical therapy to help you regain strength, flexibility, and mobility. Lifestyle changes, like maintaining a healthy weight and practising good posture, may also help prevent further spine problems in the future.
3. Can MISS treat degenerative conditions like arthritis or osteoporosis?
MISS can be effective in treating conditions that involve nerve compression, like those caused by degenerative disc disease, spinal stenosis, and some forms of arthritis. However, osteoporosis, a condition where bones become fragile, may require additional treatment options before considering surgery.
Conclusion
All in all, spine problems in older adults, while common, do not have to be debilitating. It is possible to address conditions like disc disease, spinal stenosis, and herniated discs, restoring mobility and reducing pain. Minimally invasive spine surgery presents a viable option for many, offering shorter recovery times and fewer risks compared to traditional surgeries.
If you’re dealing with spine issues and exploring treatment options, Achieve Spine And Orthopaedic Centre is here to help with minimally invasive spine surgery. Led by Dr Wu Pang Hung, Director and Senior Consultant, we offer a targeted approach to spinal health, with a focus on providing uniportal and biportal surgical solutions for patients. Our experienced team will work closely with you to find the right spine pain treatment, supporting your recovery and helping you return to your routine as quickly as possible.
Take the next step toward improved spine health and recovery. Contact us today.

Wu Pang Hung
ABOUT AUTHOR
Dr. Wu Pang Hung is an experienced orthopaedic and spine surgeon in Singapore, specialising in both uniportal and biportal endoscopic spine procedures for complex cervical, thoracic, and lumbar spinal conditions. With over 10 years in the field, he is actively involved in numerous spine societies and contributes to several international journals and textbooks. Dr. Wu has also received specialised training in spine surgery across Canada, South Korea, Japan, and Germany.
Contact Us
WHATSAPP US @+65 9746 6178
CALL US @+65 9746 6178
MAKE AN APPOINTMENT